Exercise Physiology for People with Disability: Building Strength, Safety, and Independence
Quick Answer
Exercise Physiology (EP) for people with disability focuses on building physical strength, safety, and independence through personalised and evidence-based programs. Accredited Exercise Physiologists (AEPs) work closely with clients under the NDIS, Medicare or private pathways to improve function, reduce pain, and enhance quality of life.
Introduction
Living with a disability can come with daily challenges— limited mobility, chronic pain, or reduced independence. These challenges often affect not only physical health but also mental wellbeing and social connection. Fortunately, tailored exercise programs led by Exercise Physiologists offer a powerful solution grounded in clinical care, compassion, and safety.
At Chronic Gains, we see firsthand how structured movement can restore capability and confidence in our clients across Bankstown, Sydney, and beyond. In this blog, we’ll explore how exercise physiology supports people with disability to rise, rebuild, and reclaim their health through strength, function, and empowerment.
Table of Contents
- Why This Matters
- Understanding Disability in Exercise Physiology
- Building Strength and Functional Movement Safely
- Promoting Independence Through Tailored Programs
- Addressing Barriers: Support, Mental Health, and Empowerment
- Quick Comparison Table
- Expert Insight
- Frequently Asked Questions
- Next Steps
- Author Bio
Why This Matters

- Physical inactivity among people with disability increases risk of secondary conditions like obesity, diabetes, and depression.
- Exercise physiology provides safe, adapted strategies to improve strength, mobility, and function.
- NDIS participants can access funded services to support long-term goals around independence.
- Many clients report improvements in pain, mental health, and quality of life within weeks of starting.
- The right exercise treatment reduces hospitalisations and supports ageing-in-place for people with disability.
Understanding Disability in Exercise Physiology
Defining Disability in Allied Health
Disability encompasses a wide spectrum of physical, sensory, intellectual, and neurological conditions. It may be present from birth, acquired through injury, or developed over time through chronic conditions such as multiple sclerosis, cerebral palsy, autism, or traumatic brain injury. In Exercise Physiology, we consider both the medical and functional impacts of disability.
A functional approach focuses not just on diagnosis but on how the condition affects a person’s movement, strength, and capacity to complete everyday tasks. It recognises that two individuals with the same condition may present with very different capabilities and needs.
The Role of Accredited Exercise Physiologists (AEPs)
AEPs are university-qualified allied health professionals trained to deliver clinical exercise interventions for people with chronic disease, disability, or injury. They are uniquely positioned to assess movement safely, prescribe effective treatment plans, and collaborate with multidisciplinary teams under the NDIS.
Their scope includes improving musculoskeletal strength, cardiovascular health, metabolic control, and functional independence while preventing injury or deterioration.
We use validated outcome measures such as the 6-Minute Walk Test, Berg Balance Scale, or sit-to-stand assessments to track progress.
Building Strength and Functional Movement Safely
Safe Program Design and Progression
Building strength doesn’t mean lifting heavy weights or pushing through pain. For people with disability, safety is foundational to progress. Exercise Physiologists follow strict guidelines from the American College of Sports Medicine (ACSM) and Exercise & Sports Science Australia (ESSA) when designing individualised programs.

Key safety principles include:
- Starting with bodyweight or resistance bands before progressing to weights
- Ensuring proper technique to avoid compensatory movements
- Monitoring fatigue, spasticity, and joint stability
- Integrating balance and proprioceptive training for fall prevention
- Adjusting sessions based on fatigue, pain, or neurological symptoms
Programs are updated regularly to match changes in strength, energy levels, and goals.
Evidence-Based Strength Benefits
Strengthening exercises for people with disability have been shown to:
- Increase independence in transfers and self-care
- Improve gait speed and endurance
- Reduce falls and injury risk
- Alleviate chronic pain
- Enhance bone density and postural control
According to ACSM, progressive resistance training significantly improves functional capacity in populations with neurological and musculoskeletal conditions.
Clients on our Return-to-Work page also report better work tolerance and fewer flare-ups from strength-based rehab.
If you’re unsure where to start, we’ll guide you step-by-step.

Promoting Independence Through Tailored Programs
Individualised Plans Under NDIS and Medicare
Every person deserves a plan that reflects their goals, needs, and challenges—not a one-size-fits-all routine. At Chronic Gains, we build NDIS-aligned programs that align with participant goals such as:
- Walking unassisted
- Returning to recreational activity
- Reducing reliance on carers
- Managing fatigue or pain
- Preparing for surgery or recovery
We also cater for clients accessing care under Medicare, private health or Workers Compensation, ensuring documentation, reporting and outcome tracking are tailored to the scheme.
We prioritise measurable outcomes in line with participant goals and funding reviews.
Learn how our (link to evidence-based rehabilitation services) improve day-to-day function, or explore (link to Funding Schemes page) to see available options.
Functional Outcomes and ADLs
Exercise therapy isn’t about gym performance—it’s about life performance.
By focusing on functional movements, we help clients regain ability in:
- Transfers (bed, toilet, chair)
- Walking indoors and outdoors
- Household tasks (lifting, carrying, reaching)
- Personal hygiene and dressing
- Recreational or community participation
For many clients, small gains—like walking unaided or carrying a bag—mean major improvements in autonomy and dignity.
Our Exercise Physiology assessments identify the specific movements to target for each client, ensuring efficiency and impact.
Addressing Barriers: Support, Mental Health, and Empowerment
Overcoming Fear, Stigma, and Disengagement
Many people living with disability have had negative experiences with healthcare or fitness environments. They may be hesitant to move due to fear of pain, falls, or embarrassment. Others may have disengaged due to environments that felt clinical, overwhelming or non-inclusive.
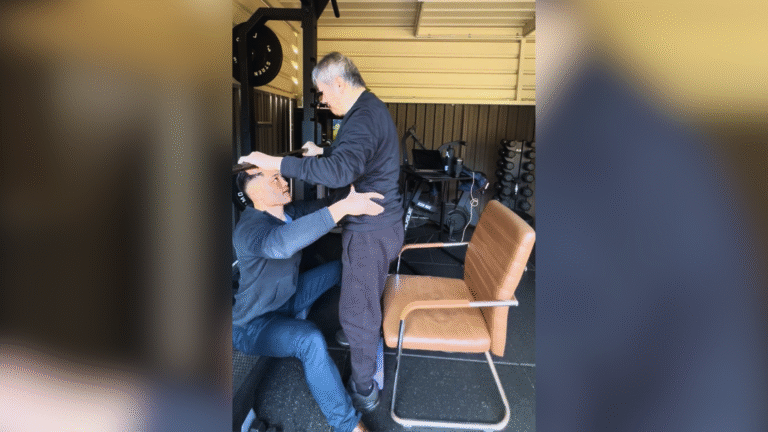
Our Exercise Physiology team takes a trauma-informed, empowering approach:
- Private, quiet spaces for clients with sensory needs
- Compassionate communication
- Collaboration with support workers or family
- Consent-based exercise plans
- A culture of encouragement and non-judgement
We believe people thrive when they feel safe, supported and seen.
Emotional and Psychosocial Support
The benefits of exercise extend well beyond the physical. For people with disability, it often serves as:
- A form of routine and structure
- A pathway to social reconnection
- A tool for emotional regulation and mood boosting
- A confidence-building experience
Our clinicians integrate motivational interviewing and psychosocial support into every session.
You can also read what our clients say about their outcomes on our Testimonials page or see how Workers Compensation rehabilitation programs support both physical and emotional health.
Quick Comparison Table
| Allied Health Role | Focus | Approach for Disability |
|---|---|---|
| Exercise Physiologist (EP) | Functional movement, strength, prevention | Tailored exercise, goal tracking, NDIS funded |
| Physiotherapist | Diagnosis, pain management, rehab | Often early-stage rehab, shorter intervention |
| Occupational Therapist (OT) | Daily living tasks, environmental adaptation | Focus on ADL tools, home/environment adjustment |
Expert Insight
Pro Tip: According to ACSM and ESSA guidelines, exercise interventions for people with neurological or physical disability should begin at low intensity, prioritising function and safety, and gradually progress toward building strength and endurance over 6–12 weeks.
Frequently Asked Questions
Q: Can people with disability safely exercise?
A: Yes. With supervision from an Exercise Physiologist, exercise is not only safe—it’s essential. Programs are tailored to the condition, risk level, and ability of the individual.
Q: Is Exercise Physiology covered under NDIS?
A: Absolutely. NDIS participants can access Exercise Physiology services through Capacity Building funding. We help with documentation and reporting to support goals.
Q: What if the person has pain or fatigue?
A: Programs are adapted daily to account for fatigue, pain or flare-ups. The goal is to move within safe limits, promote recovery, and avoid worsening symptoms.
Q: How long before results are seen?
A: Many clients report improvement in energy, mobility or pain within 4–6 weeks. Strength and functional gains often appear by 8–12 weeks with consistency.
Next Steps
If you or someone you support is living with disability and ready to take back control of your movement and health, we’re here to help. Our Exercise Physiology team in Bankstown and Sydney provides clinical, compassionate support tailored to your goals.
Book an initial assessment today and see how movement can change your life.
Author Bio
Chronic Gains Exercise Physiology is a trusted provider of tailored, evidence-based Exercise Physiology services in Bankstown and Sydney. We specialise in helping people living with disability, chronic conditions, and injury to rebuild strength, function, and confidence.
Our team provides compassionate care through the NDIS, CDM (Chronic Disease Management), Workers Compensation, CTP (Compulsory Third Party) claims, DVA (Department of Veterans’ Affairs).