Supporting NDIS Participants’ Goals: Focus, Progress, and Personalisation
Introduction
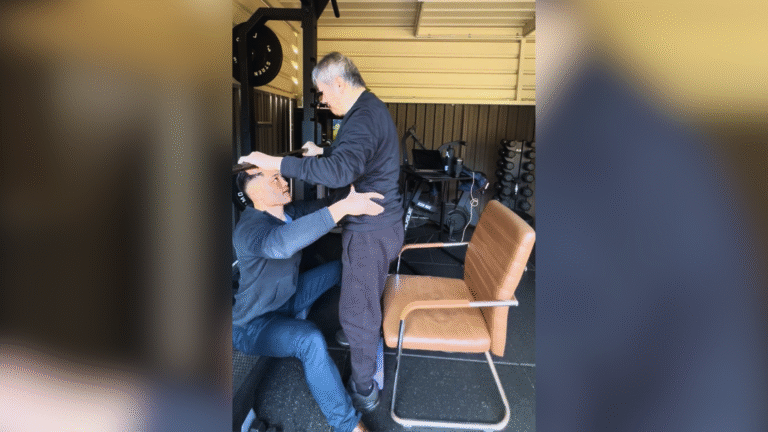
At Chronic Gains, we know that no two journeys are the same. Whether you’re part of the local Bankstown community or looking for trusted support across Sydney, you deserve individualised care that’s grounded in empathy, expertise, and real-world experience.
For many National Disability Insurance Scheme (NDIS) participants, exercise isn’t simply about fitness—it’s about reclaiming your strength, improving daily function, and achieving goals that truly matter to you.
But how do you make sure your exercise plan isn’t generic? How do you ensure it’s not just “movement” but “movement as medicine” that genuinely supports your personal goals?
In this article, we’ll explore the importance of focused, personalised, and goal-directed exercise for NDIS participants. We’ll show you how structured plans, progress tracking, and individualised care can help you move with purpose, confidence, and safety—so you can empower your health without the guesswork.
Why Goals Matter: Moving Beyond Generic Exercise

When you hear “exercise,” what comes to mind? For many, it’s a vague idea: “get stronger,” “get fitter,” or “lose weight.” But these general aims often fail to motivate, especially when you’re managing a chronic condition or disability. For NDIS participants, goals aren’t just helpful—they’re essential.
A meaningful goal is personal. It might be being able to transfer safely from bed to chair without assistance. Walking to the corner shop without fatigue. Playing with your kids on the floor and getting up without fear. These aren’t just activities—they’re steps toward independence, dignity, and improved quality of life.
As Accredited Exercise Physiologists (AEPs), we’re trained to turn these real-life goals into clear, structured plans. We follow evidence-based approaches drawn from resources like the American College of Sports Medicine (ACSM) guidelines and Exercise & Sports Science Australia (ESSA) best-practice principles.
For example, ACSM emphasises that exercise prescription should always be individualised—matching goals, medical history, current abilities, and preferences. That means there’s no “one-size-fits-all” template.
Why does this matter?
- It reduces frustration by setting realistic, meaningful targets.
- It enhances motivation because goals are personal and relevant.
- It promotes safety, by considering health conditions, medications, and mobility.
- It respects your choices and empowers you to lead your care.
In practice, this means working together to define SMART goals—Specific, Measurable, Achievable, Relevant, and Time-bound. But it also means treating you as a person, not a checkbox.
Personalisation in Practice: Case Examples and Scenarios
What does this actually look like? Let’s talk about Sarah.
Sarah is 32, living with multiple sclerosis (MS). She’s an NDIS participant who came to us because she wanted to feel less fatigued during daily chores and regain some confidence in her balance.
We didn’t start with generic gym exercises. Instead, our initial assessment included:
- A detailed medical history and discussion of MS symptoms (e.g. heat sensitivity, spasticity)
- Balance testing using evidence-based protocols
- Mobility assessments
- Collaborative goal setting
Together, we set two goals:
- Improve balance to reduce fall risk.
- Increase endurance to manage housework without excessive fatigue.
Her structured plan included:
- Tailored resistance exercises for lower-limb strength.
- Balance drills using dual-task activities (so she can better handle real-world challenges like talking while walking).
- Low-intensity aerobic sessions, carefully monitored to avoid overheating and exacerbating symptoms.
After 12 weeks, Sarah reported fewer stumbles, more confidence in moving around her home, and better energy management. Another example is Mark, who lives with autism. Mark’s main goal was social participation—he wanted to feel confident joining a local walking group.
We designed sessions to:
- Gradually increase walking distances and tolerance.
- Practice social scenarios in a safe environment.
- Include sensory considerations, like preferred quiet times and familiar routes.
After three months, Mark felt ready to join his group and made new connections, showing that exercise isn’t just physical, but social and emotional too.

These examples show what personalised care really is:
- Listening first
- Understanding individual goals and barriers
- Designing plans that support that person’s life
- Names and details have been changed for privacy.
Focus and Structure: Why “No Guesswork” Matters

If you’re an NDIS participant—or supporting one—you know how easy it is to feel overwhelmed by conflicting advice. One professional says “do more cardio,” another says “lift weights,” someone else says “just walk.” It can leave you thinking: Which is right for me?
At Chronic Gains, we believe in no guesswork. That means:
- Comprehensive initial assessment
- Evidence-based exercise prescription
- Clear documentation of your goals and progress
- Ongoing review and adjustments
This approach is supported by ACSM’s core exercise prescription principles:
Exercise plans should be progressive, individualised, and based on careful screening and evaluation.
It’s not just best practice—it’s essential for safety.
For example, some NDIS participants have conditions where certain movements should be modified or avoided:
- Joint hypermobility? Avoid excessive end-range stretches without control.
- Cardiovascular disease? Monitor intensity carefully, using validated scales or heart rate guidelines.
- Autism or sensory processing differences? Modify environments and cues to reduce distress.
A structured plan prevents injury, frustration, and wasted time. It also creates accountability.
Imagine walking into a session knowing:
- What you’re doing
- Why you’re doing it
- How it connects to your goals
That clarity is empowering. It builds trust in the process and your own body.
Tracking Progress: A Motivational Tool, Not a Test
Some people worry that “tracking progress” means judgment or pressure. At Chronic Gains, we see it differently.
Progress tracking is about celebrating wins—big and small. It helps us see what’s working, what needs adjusting, and how far you’ve come.
Consider these examples:
- Functional tests: Timed Up and Go (TUG) to see improvements in safe transfers.
- Strength tests: Number of chair stands in 30 seconds.
- Balance assessments: Reductions in sway or improvements in single-leg stance.
- Patient-reported outcomes: Fatigue scales, quality-of-life questionnaires.
We don’t use these to grade you, but to empower your health.
As exercise physiologists, we know that sometimes the wins are subtle but vital:
- Less pain when getting out of bed.
- Fewer rests are needed while shopping.
- Being able to lift your grandchild safely.
These stories matter. They’re why we love our work.
Collaboration with Your Care Team

Another strength of personalised exercise for NDIS participants is that it doesn’t exist in isolation.
We often work with:
- Physiotherapists
- Occupational therapists
- Support coordinators
- Family and carers
This ensures the plan is aligned with all your goals—from mobility to daily living skills to community participation.
For instance:
- An OT might highlight bathroom transfers as a priority—we’ll include relevant strength and balance training.
- A physio might identify gait pattern issues—we’ll coordinate exercises to reinforce their work.
- A support worker might share barriers like transport issues—we’ll adapt home-based or community-based options.
This is support that makes sense. It ensures everyone’s on the same page, reducing confusion and duplication. It also reduces your burden—you shouldn’t have to be the one coordinating all the details.
Safety First: Evidence-Based Principles
At Chronic Gains, our approach is grounded in the best available evidence.
We draw on:
- American College of Sports Medicine guidelines
- ESSA recommendations
- Relevant clinical guidelines for specific conditions
This means every exercise plan:
- Includes appropriate screening (e.g. PAR-Q+, ACSM risk stratification).
- Considers comorbidities and medication effects.
- Follows proven progression principles.
- Balances challenge with safety.
For example, ACSM guidelines highlight that:
Physical inactivity is a major contributor to chronic disease and functional decline—but exercise must be tailored to the individual to reduce risk and maximise benefit.
That’s why we don’t just hand out a generic program.
Instead, we use assessments to guide prescription:
- Mobility, strength, and balance testing
- Cardiovascular risk screening
- Pain and fatigue levels
- Functional needs in daily life
This is how movement as medicine works in practice.
Empowerment Through Education
Finally, our goal is always to empower you.
We don’t just want to lead sessions—we want to help you understand your body, your program, and your progress.
Education might include:
- Explaining why certain exercises are chosen.
- Teaching self-monitoring tools (e.g. RPE scales, heart rate zones).
- Helping you identify early signs of fatigue or overuse.
- Reviewing techniques to maintain independence long-term.
Because it’s your journey. Our role is to give you tools, confidence, and knowledge.
Supporting NDIS participants isn’t about ticking boxes or offering generic classes. It’s about person-centred care that respects individual goals, needs, and strengths. At Chronic Gains, we believe in reclaiming your strength through structured, evidence-based, and compassionate exercise. We’re here to listen, plan, guide, and celebrate every step with you. Contact us today if you’re ready to move with purpose and confidence. We’d be honoured to support you on that journey.