Why We Choose Specific Exercises for NDIS Clients
Introduction
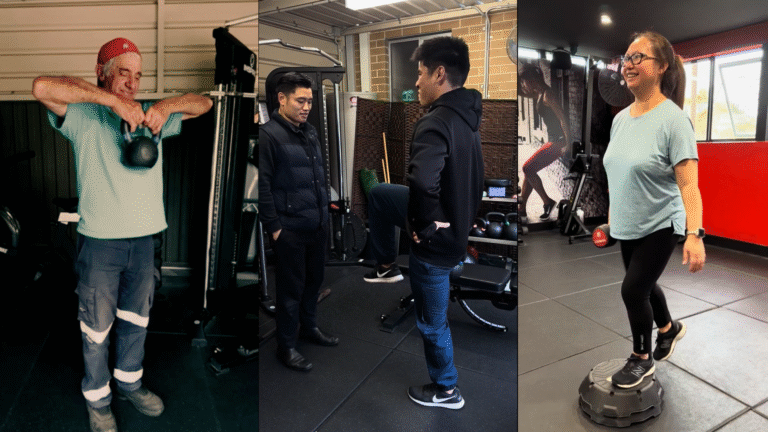
At Chronic Gains, we know that exercise isn’t just about movement—it’s about movement as medicine. For our clients in Bankstown and right across Sydney, this philosophy shapes every decision we make.
For NDIS participants, choosing the right exercises is critical. It’s not about a “one-size-fits-all” program or just getting people moving. It’s about reclaiming strength, improving independence, and working toward personal goals—safely, effectively, and with individualised care.
But what does it actually mean to choose exercises specifically for you? Why don’t we just hand out generic workouts or tell everyone to “walk more”?
In this article, we’ll explain why exercise prescription for NDIS participants demands focus, personalisation, and evidence-based planning. We’ll show you how your goals, health conditions, and daily needs shape our approach—so there’s no guesswork and only support that makes sense.
Why “Specific” Beats “Generic”: The Importance of Individualised Care
Have you ever been told to “just exercise more” without any guidance? It’s frustrating—and for many people, dangerous. For NDIS participants living with diverse health conditions and abilities, generic advice can lead to:
- Increased risk of injury
- Frustration and loss of motivation
- Feeling ignored or misunderstood
- Wasted time and money
At Chronic Gains, we prioritise individualised care. As Accredited Exercise Physiologists (AEPs), we’re trained to assess your medical history, current ability, and personal goals. We use evidence-based guidelines—like those from the American College of Sports Medicine (ACSM) and Exercise & Sports Science Australia (ESSA)—to make sure our exercise choices are both safe and effective.
So what makes an exercise “specific” for you?
It’s one that:
- Matches your goals and daily life needs
- Accounts for your health conditions and medications
- Adapts to your physical ability and mobility
- Supports your motivation and enjoyment
For example, let’s say your goal is to transfer safely from a wheelchair to the bed. You don’t need generic “leg day” exercises from the gym. You need targeted strength training for specific muscle groups, functional transfer practice, and balance work tailored to your environment. That’s the power of specificity—it’s about you.
Understanding the Assessment: The Foundation of Specific Exercise
Before prescribing anything, we listen. That starts with a comprehensive assessment.
- Health and medical history: What conditions do you live with? What medications affect your movement or heart rate? Do you have pain, fatigue, or other barriers?
- Functional goals: What really matters to you? Not vague “fitness,” but personal goals like gardening, going shopping, playing with family, or living more independently.
- Mobility and strength testing: Using safe, evidence-based tools (like sit-to-stand tests, balance assessments, or gait analysis) to find your starting point.
- Cardiovascular screening: Including ACSM risk stratification to ensure you’re safe for certain intensities and types of exercise.
- Sensory and cognitive considerations: Especially important for participants with autism, intellectual disability, or brain injuries.
This assessment isn’t about labelling you—it’s about understanding you. It means the difference between a program that frustrates you and one that genuinely empowers you.
The Role of Goals: Anchoring Exercise Choices in Your Life
Goals are the compass for exercise prescription. We don’t pick exercises at random. Every choice has to serve your goals. Consider these examples (without using client avatars, just common scenarios):
A participant with multiple sclerosis wants to reduce falls.
- We prioritise balance exercises, lower-limb strength, and dual-task training (like balancing while doing another task).
- We manage intensity carefully to avoid fatigue or heat-related symptoms.
A participant with autism wants to join a local walking group.
- We gradually build walking tolerance in quiet environments.
- We include sensory-friendly options and social rehearsal.
A participant recovering from stroke wants to improve transfers.
- We focus on functional leg strength, trunk control, and safe transfer practice.
- We adapt for any one-sided weakness or spasticity.
A participant with chronic pain wants to return to gardening.
- We introduce graded exposure to squatting and lifting.
- We include pacing strategies and pain education.
In all these cases, exercise choices are goal-driven. This is how we turn “exercise” into chronic condition support that actually changes lives.
Evidence-Based Prescription: No Guesswork
At Chronic Gains, there’s no guesswork. We use evidence-based guidelines to choose exercise type, intensity, duration, and progression.
For example, ACSM recommends that exercise plans should be:
- Individualised: Based on screening and goals
- Progressive: Gradually increasing challenge to improve safely
- Specific: Targeting the desired outcome
- Safe: Including appropriate monitoring
We also follow principles like FITT:
- Frequency: How often you exercise.
- Intensity: How hard you work, which we might measure with heart rate, RPE (Rating of Perceived Exertion) scales, or talk tests.
- Time: How long each session lasts.
- Type: The kind of exercise, from strength to balance to cardio.
For example:
- Someone with cardiovascular risk might need careful intensity monitoring.
- Someone with joint hypermobility might avoid extreme stretching without control.
- Someone with sensory processing differences might need quieter spaces or simpler cues.
These aren’t “extras”—they’re essential.
Progression: Adapting Over Time
Your needs and abilities change. So should your program. We don’t choose exercises once and forget them. We constantly reassess and adapt. For instance:
- A participant who initially needs assistance for sit-to-stand might progress to unassisted reps, then weighted versions.
- A balance drill on firm ground can progress to unstable surfaces.
- A walking goal might start with 5 minutes indoors and progress to community walks.
This progression is key to avoiding plateaus, keeping motivation high, and continuing to improve function. It’s also safer—by avoiding sudden jumps in difficulty that can cause injury or frustration.
Functional Relevance: Exercises That Translate to Daily Life

We choose exercises that matter.
Functional exercise means training movements you actually use in daily life:
- Sit-to-stand: For getting out of chairs and beds
- Step-ups: For stairs and curbs
- Carrying: For groceries or bags
- Balance drills: For reducing falls risk
- Rotational strength: For reaching and turning
This isn’t about making you a bodybuilder or an elite athlete. It’s about making daily life easier and safer. For NDIS participants, that’s not a bonus—it’s the goal.
Safety Considerations: Reducing Risk
Safety is non-negotiable.
We choose exercises carefully to reduce risk of:
- Falls
- Joint injuries
- Cardiovascular events
- Overuse injuries
That means:
- Thorough screening
- Monitoring vital signs or perceived exertion
- Educating you on proper form
- Adapting for pain or fatigue levels
We also consider how medications might affect exercise tolerance (e.g. beta-blockers reducing heart rate response). And we help you learn self-monitoring strategies so you can continue safely outside of our sessions.



Motivation and Enjoyment: Supporting Adherence
Exercise isn’t helpful if you don’t want to do it. We talk with you about:
- Preferences for location (clinic, home, community)
- Equipment you have access to
- Social factors (solo vs group sessions)
- Sensory comfort (noise levels, lighting)
We want you to look forward to sessions—not dread them. Because consistency drives results.
Your exercise program doesn’t stand alone. We often work with:
- Physiotherapists: Aligning on mobility and gait goals.
- Occupational therapists: Supporting ADLs (Activities of Daily Living) like dressing or showering.
- Speech therapists or psychologists: Ensuring cognitive load or communication needs are respected.
- Support workers and family: Helping implement plans at home.
This teamwork ensures your exercise prescription is part of a holistic, coordinated approach. That’s support that makes sense.
Education and Empowerment: Giving You the Tools
We don’t just tell you what to do. We teach you why. This includes:
- Explaining exercise choices
- Teaching self-monitoring (e.g. RPE scales)
- Addressing fears or myths about exercise
- Helping you plan for setbacks or changes
Our goal is to help you reclaim your strength and become as independent as possible. Because exercise isn’t something we do to you—it’s something we do with you. That’s how we empower your health.
Conclusion
At Chronic Gains, we don’t believe in generic programs. We believe every NDIS participant deserves individualised, evidence-based exercise that truly supports their goals. That means thorough assessment, specific exercise choices, ongoing progression, and holistic collaboration. Because exercise isn’t just movement. It’s medicine. It’s your path to greater strength, independence, and confidence. We’re honoured to walk that path with you. If you’re ready for personalised support that makes sense, we’d love to hear your story. Contact us today!